Introduction
As a laparoscopic surgeon, one of the most commonly performed and highly successful procedures I encounter is the laparoscopic cholecystectomy — the minimally invasive removal of the gallbladder. This procedure has revolutionized the management of gallbladder diseases, offering patients faster recovery, less pain, and reduced scarring compared to traditional open surgery.
In this detailed blog post, I will walk you through every critical aspect of laparoscopic cholecystectomy, including its indications, advantages, benefits over open cholecystectomy, the surgical process, potential complications, and patient recovery.
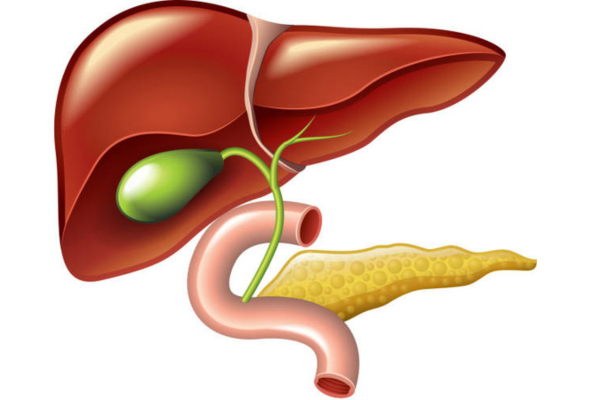
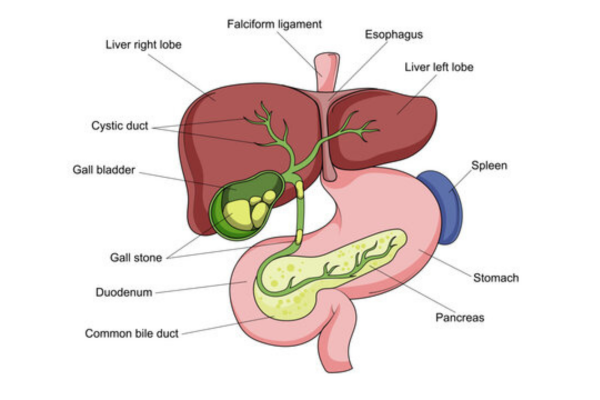
Understanding the Gallbladder
Before we dive into the procedure, let’s understand the organ in question.
The gallbladder is a small, pear-shaped organ located under the liver. It stores and concentrates bile, a digestive fluid produced by the liver, which helps in the digestion of fats. When we eat fatty foods, the gallbladder contracts and releases bile into the small intestine through the bile ducts.
When the gallbladder becomes diseased—most commonly due to gallstones—it may need to be removed. Gallstones can cause inflammation, infection, or blockages that result in severe pain and complications.
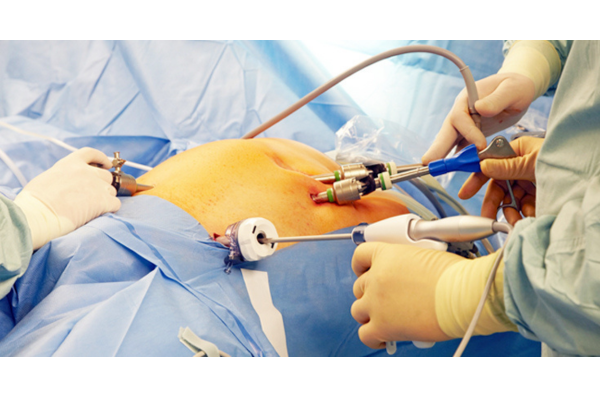
What is Laparoscopic Cholecystectomy?
Laparoscopic cholecystectomy is a minimally invasive surgery used to remove the gallbladder. It involves making a few small incisions in the abdomen through which a laparoscope (a tiny camera) and specialized surgical tools are inserted.
The camera projects images onto a screen, allowing the surgeon to view the internal organs in real-time and perform precise surgical maneuvers. The gallbladder is dissected and carefully removed through one of the small incisions.
Indications for Laparoscopic Cholecystectomy
As a surgeon, we don’t remove the gallbladder unless necessary. Here are the main indications for this surgery:
1. Symptomatic Gallstones (Cholelithiasis)
- Recurrent right upper abdominal pain
- Pain after fatty meals
- Nausea or vomiting
2. Acute Cholecystitis
- Inflammation of the gallbladder due to gallstone obstruction
- Fever, tenderness, elevated white blood cell count
3. Biliary Colic
- Intermittent, cramping pain caused by temporary blockage of the bile duct
4. Choledocholithiasis
- Gallstones in the common bile duct
- May require endoscopic stone removal before cholecystectomy
5. Gallbladder Polyps
- Polyps larger than 1 cm or symptomatic polyps
6. Gallstone Pancreatitis
- Inflammation of the pancreas caused by gallstones blocking the bile duct
7. Porcelain Gallbladder
- Calcified gallbladder wall, associated with cancer risk
8. Gallbladder Dyskinesia
- Abnormal gallbladder emptying with confirmed low ejection fraction on HIDA scan
Advantages of Laparoscopic Cholecystectomy
Laparoscopic cholecystectomy has become the gold standard for gallbladder removal due to several key benefits:
1. Minimally Invasive
- Only 3–4 small incisions (0.5–1 cm)
- Less trauma to the body

2. Less Postoperative Pain
- Reduced pain compared to large incision of open surgery
3. Faster Recovery
- Most patients return to daily activities in 1–2 weeks
- Less time off work
4. Shorter Hospital Stay
- Often performed as a day-care or 1-day stay surgery
5. Better Cosmetic Outcome
- Small scars, often nearly invisible after healing
6. Lower Risk of Infection
- Smaller incisions reduce the risk of wound infections
7. Reduced Blood Loss
- Minimally invasive tools help minimize bleeding
How is Laparoscopic Cholecystectomy Performed?
Preoperative Preparation
- Patient evaluation (blood tests, ultrasound, ECG, etc.)
- Fasting for 6–8 hours
- Informed consent
Anesthesia
- Performed under general anesthesia
Surgical Steps
- Creation of Pneumoperitoneum:
- CO₂ gas is introduced into the abdomen to create working space
- Insertion of Trocars:
- Usually 3 or 4 trocars are placed:
- Umbilical port for the laparoscope
- Two to three working ports for instruments
- Usually 3 or 4 trocars are placed:
- Dissection of Gallbladder:
- Identify and clip cystic duct and artery
- Dissect gallbladder from liver bed
- Gallbladder Removal:
- Removed via umbilical port
- Closure:
- Gas is released
- Incisions are closed with absorbable sutures or skin glue
Duration:
- Average time: 30 to 90 minutes
Comparison with Open Cholecystectomy
| Feature | Laparoscopic Cholecystectomy | Open Cholecystectomy |
|---|---|---|
| Incision | Small (0.5–1 cm) | Large (10–15 cm) |
| Pain | Minimal | More significant |
| Recovery Time | 1–2 weeks | 4–6 weeks |
| Hospital Stay | 1 day or same-day discharge | 3–5 days |
| Scar | Minimal | Prominent |
| Risk of Infection | Lower | Higher |
| Return to Work | Sooner | Delayed |
| Surgical View | Magnified view | Direct vision |
Laparoscopic surgery is clearly superior in most elective cases unless contraindicated.
Contraindications for Laparoscopic Cholecystectomy
Though highly effective, certain situations may necessitate open surgery or delay laparoscopic intervention:
Absolute Contraindications
- Uncontrolled bleeding disorders
- Severe cardiopulmonary disease prohibiting general anesthesia
Relative Contraindications
- Previous upper abdominal surgeries (due to adhesions)
- Severe inflammation or gangrene of the gallbladder
- Suspected gallbladder cancer
- Large gallstones that can’t be removed laparoscopically
Potential Complications
Though complications are rare, it’s crucial to be aware of them:
1. Bile Duct Injury
- Serious but rare (0.3–0.5%)
- May require further surgery
2. Bleeding
- From liver bed or vessels
3. Infection
- Wound or intra-abdominal abscess
4. Bile Leak
- From cystic duct or small accessory ducts
5. Conversion to Open Surgery
- In 2–5% of cases due to poor visibility or complications
6. Deep Vein Thrombosis
- Prevented with early mobilization
Recovery After Laparoscopic Cholecystectomy
Immediate Post-op Care
- Observation for a few hours
- Light oral fluids after 4–6 hours
Diet
- Resume regular diet gradually
- Some patients may need to avoid high-fat foods for a few weeks
Activity
- Light activities within 2–3 days
- Avoid heavy lifting for 2 weeks
Follow-up
- Usually within 7–10 days for wound check
Long-Term Outcome
- Most patients live normally without a gallbladder
- Digestion is not significantly affected
Benefits to Patients
From a patient’s perspective, laparoscopic cholecystectomy offers:
- Improved Quality of Life: Relief from chronic pain and discomfort
- Quick Resumption of Daily Routine: Return to work and family duties faster
- Low Recurrence Risk: Once removed, gallstones don’t recur
- Reduced Hospital Costs: Shorter stays and less use of resources
- Peace of Mind: Minimal scarring, better healing, fewer complications
Surgeon’s Perspective: Why Laparoscopy is the Preferred Choice
As a surgeon, I prefer laparoscopy because:
- The magnified camera view offers better visualization of delicate structures.
- Precision dissection is easier and safer.
- Blood loss is minimal, and anatomy is clearly defined.
- Patient satisfaction is much higher due to the fast recovery and minimal scars.
Even in complex cases, laparoscopy is often feasible with expertise and careful planning.

Conclusion
Laparoscopic cholecystectomy has become the standard of care for gallbladder removal due to its safety, effectiveness, and numerous benefits over open surgery. With modern instruments, experienced surgical teams, and patient education, outcomes have dramatically improved.
For patients suffering from gallbladder-related symptoms, this minimally invasive approach offers a quick, safe, and permanent solution. As a laparoscopic surgeon, I can confidently say that this procedure has transformed the way we treat gallbladder diseases—and improved countless lives in the process.
